References
[1] J.A Muir Gray. Evidence-based Healthcare: How to Make Health Policy and Management Decisions. Churchill Livingston, 1997
[2] L Sackett, William MC Rosenberg, JA Muir Gray, R Brian Haynes, W Scott Richardson. Editorial from the British Medical Journal. BMJ 1996; 312: 71-2
[3] Sim I, Gorman P, Greenes R, Haynes RB, Kaplan B, et al. Clinical decision support systems for the practice of evidence-based medicine. Journal of the American Medical Informatics Association 2001; 8(6):527-34
[4] Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ 2001;323:334-6
[5] Rockville (MD): US Department of Health and Human Services.Clinical Practice Guideline No.1: acute pain management: operative or medical procedures and trauma. Agency for Health Care Policy and Research; 1993. AHCPR Publication No. 92-0023
[6] Scottish Intercollegiate Guidelines Network (SIGN). Methodology Review Group. Report on the review of the method of grading guideline recommendations. Edinburgh; SIGN: 1999
[7] The Canadian Guide to Clinical Preventive Health Care. Recommendations by Strength of Evidence. Accessed March 12, 2003
[8] US Preventive Services Task Force. Translating evidence into recommendations. Accessed March 6, 2003
[9] Field MJ, Lohr KN (Editors). Clinical practice guidelines: directions for a new program. Committee to Advise the Public Health Service on Clinical Practice Guidelines
[10] Scottish Intercollegiate Guidelines Network (SIGN). Clinical guidelines: criteria for appraisal for national use. Edinburgh; SIGN: 1995
[11] Appraisal of Guidelines, Research and Evaluation for Europe website. http://www.agreecollaboration.org/
[12] SIGN 50:A guideline developers' handbook website. http://www.sign.ac.uk/guidelines/fulltext/50/index.html
[13] Quaglini S, Dazzi L, Gatti L, Stefanelli M, Fassino C, Tondini C. Supporting tools for guideline development and dissemination. Artificial Intelligence in Medicine 1998; 14:119-137
[14] Quaglini S, Stefanelli M, Cavallini A, Micieli G, Fassino C, Mossa C. Guideline-based Careflow Systems. Artificial Intelligence in Medicine 2000; 20(1) 5-22
[15] Ciccarese P, Caffi E, Boiocchi L, Quaglini S, Stefanelli. A Guideline Management System. Medinfo 2004, IOS Press, pag. 28 - 32 (2004)
[16] A. A. Boxwala, M. Peleg, S. W. Tu, O. Ogunyemi, Q. Zeng, D. Wang, V. L. Patel, R. A. Greenes, E. H. Shortliffe. GLIF3: A Representation Format for Sharable Computer-Interpretable Clinical Practice Guidelines. Journal of Biomedical Informatics (JBI), 37 (3): 147-161 2004.
[17] S. W. Tu, M. A. Musen. The EON Model of Intervention Protocols and Guidelines. 1996 AMIA Annual Fall Symposium, Washington, D.C., 587-591. Hanley & Belfus, 1996.
[18] Bury J., Fox J., Sutton D. The PROforma guideline specification language: progress and prospects. Proceedings of the First European Workshop, Computer-based Support for Clinical Guidelines and Protocols (EWGLP 2000), Leipzig 13-14 Nov. 2000.
[19] Sutton DR, Fox J. The Syntax and Semantics of the PROforma guideline modelling language. J Am Med Inform Assoc. 2003 Sep-Oct;10(5):433-43.
[20] Purves IN, Sugden B, Booth N, Sowerby M. The PRODIGY project - the iterative development of the release one model. Proc AMIA Symp. 1999;:359-63.
[21] Johnson P, Tu S, Jones N. Achieving reuse of computable guideline systems. Medinfo. 2001;10(Pt 1):99-103.
[22] Shahar, Y., Miksch, S., and Johnson, P. The Asgaard project: A task-specific framework for the application and critiquing of time-oriented clinical guidelines. Artificial Intelligence in Medicine (14): 29-51, 1998.
[23] J. R. Campbell, S. W. Tu, J. G. Mansfield, J. I. Boyer, J. McClay, C. Parker, P. Ram, S. M. Scheitel, K. McDonald. The SAGE Guideline Model: A Knowledge Representation Framework for Encoding Interoperable Clinical Practice Guidelines. 2003.
[24] P. Ram, D. Berg, S. W. Tu, J. G. Mansfield, Q. Ye, R. Abarbanel. Executing Clinical Practice Guidelines using the SAGE Execution Engine. 2003.
[25] Peleg M, Tu S, Ciccarese P, Kumar A, Quaglini S, Stefanelli M et al. Comparing models of decision and action for guideline-based decision support: a case-study approach. JAMIA 2003; vol. 1 ,n.10, 52-68
[26] P.A. de Clercq, J.A. Blom, H.H. Korsten and A. Hasman. Approaches for creating computer-interpretable guidelines that facilitate decision support. Artif Intell Med. 2004; 31(1): 1-27
[27] Barner E. S., Baker S, Funkhouser E. et al. Do local opinion leaders augment hospital quality improvement efforts? A randomized trial to promote adherence to unstable angina guidelines. Med Care 2003; 41; 420-431.
[28] Eccles M., McColl E. et al. Effect of computerized evidence based guidelines on management of asthma and angina in adults in primary care: cluster randomised controlled trial. BMJ 2002 vol. 325.
[29] Lazarsfeld PF, Merton RK. Friendship as social process: a substantive and methodological analysis. In Berger M, et al. (eds.). Freedom and Control in Modern Society. New York: Octagon, 1964.
[30] D.B. Fridsma ,J.H. Gennari, M.A. Musen. Making generic guidelines site-specific. Proc. AMIA 1996, 597-601.
[31] Peleg M, Tu S, Bury J, Ciccarese P. et al. Comparing models of decision and action for guideline-based decision support: a case-study approach. JAMIA 2003; vol. 1 ,n.10, 52-68
[32] Clercq, P.A. de; Blom, J.A.; Korsten, H.H.M.; Hasman, A. Approaches for creating computer-interpretable guidelines that facilitate decision support. Art. Intell. Med. 31, nr. 1, 2004, pp. 1-27. SPS-40 [06.01]
[33] Shahar, Y., Miksch, S., and Johnson, P. The Asgaard project: A task-specific framework for the application and critiquing of time-oriented clinical guidelines. Artificial Intelligence in Medicine (14): 29-51, 1998.
<
[34] Seyfang A, Kosara R, Miksch S. Asbru's Reference Manual, Version 7.3. Vienna University of Technology, Institute of SoftwareTechnology, Vienna; 2002. Report No.: Asgaard-TR-2002-1.
[35] Tu SW, Musen MA. A Flexible Approach to Guideline Modeling. Proc AMIA Symp. 1999:420-424.
[36] Tu SW, Musen MA. From Guideline Modeling to Guideline Execution: Defining Guideline-Based Decision-Support Services. Proc AMIA Annu Symp. 2000:863-867.
[37] Tu SW, Musen MA. Modeling Data and Knowledge in the EON Guideline Architecture. Proc Medinfo: 280-284.
[38] Peleg M, Boxwala A, Ogunyemi O, et al. GLIF3: The Evolution of a Guideline Representation Format. Proc AMIA Annu Fall Symp. 2000:645-649.
[39] Hripcsak G, Ludemann P, Pryor TA, Wigertz OB, Clayton PD. Rationale for the Arden Syntax. Comput Biomed Res. 1994;27(4):291-324.
[40] Schadow G, Russler DC, Mead CN, McDonald CJ. Integrating Medical Information and Knowledge in the HL7 RIM. Proc AMIA Annu Fall Symp. 2000:764-768.
[41] Ogunyemi O, Zeng Q, Boxwala A. Object-oriented guideline expression language (GELLO) specification. Brigham and Women's Hospital, Harvard Medical School, 2002. Decision Systems Group Technical Report DSG-TR-2002-001.
[42] Johnson PD, Tu SW, Booth N, Sugden B, Purves IN. Using Scenarios in Chronic Disease Management Guidelines for Primary Care. Proc AMIA Annu Fall Symp. 2000:389-393.
[43] Grosso WE, Eriksson H, Fergerson R, Gennari JH, Tu SW, Musen MA. Knowledge Modeling at the Millennium (The Design and Evolution of Protege-2000). Proc 12th Banff Knowledge Acquisition for Knowledge-Based Systems Workshop. Canada; 1999:7-4-1 to 7-4-36.
[44] Johnson P, Tu S, Jones N. Achieving reuse of computable guideline systems. Medinfo. 2001;10(Pt 1):99-103.
[45] Fox J, Johns N, Rahmanzadeh A, Thomson R. PROforma: A method and language for specifying clinical guidelines and protocols. Proc Medical Informatics Europe; Amsterdam; 1996.
[46] Fox J, Das S. Safe and Sound. In: Safe and Sound: AAAI Press; 2000.<(p>
[47] De Clercq PA, Blom JA, Hasman A, Korsten HHM. Design and implementation of a framework to support the development of clinical guidelines. Int J Med Inf 2001;64(2- 3):285-318.
[48] De Clercq PA, Blom JA, Hasman A, Korsten HH. GASTON: an architecture for the acquisition and execution of clinical guideline-application tasks. Med Inform Internet Med. 2000 Oct-Dec;25(4):247-63.<(p>
[49] Terenziani P, Mastromonaco F, Molino G, Torchio M. Executing clinical guidelines: temporal issues. Proc AMIA Symp. 2000;:848-52.
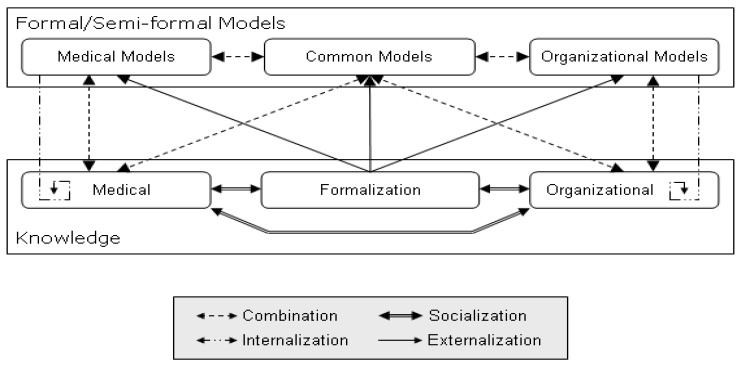
[50] Stefanelli M. The socio-organizational age of artificial intelligence in medicine. Artificial Intelligence in Medicine 2001;23:25–47.
[51] Stefanelli M. Knowledge management to support performance based medicine. Methods of Information in Medicine 2002;41:36–43.
[52] URL: http://www.wfmc.org/
[53] Coiera E. When communication is better than computation. Journal of American Medical Informatics Association 2000;7:277–86.
[54] Fox MS, Gruninger M. Enterprise modeling. AI Magazine 1998;(Fall):109–21.
[55] S. Quaglini, S. Panzarasa, A. Cavallini, G. Micieli, C. Pernice, M. Stefanelli. Smooth Integration of Decision Support into an Existing Electronic Patient Record. Artificial Intelligence in Medicine ,ed Silvia Miksch; Jim Hunter; Elpida Keravnou (Eds.), pag. 89 - 93, (2005)
[56] S. Panzarasa, R. Bellazzi, C.Larizza, M. Stefanelli. A careflow management system for chronic patients. MedInfo 2004 ,ed Fieschi/Coiera e Yu-Chan Jack Li, pag. 773 - 777, (2004).
[57] Johnson PD, Tu SW, et al. A virtual medical record for guideline-based decision support. Proc AMIA Symp. 2001; pp. 294-298.
[58] Paolo Ciccarese, Ezio Caffi, Silvana Quaglini, Mario Stefanelli. Architectures and Tools for innovative Health Information Systems: the Guide Project. International Journal of Medical Informatics, vol. 74 ,n. ,pag. 553-562 ,(2005)
[59] Nonaka I, Takeuchi H. The knowledge-creating company. Oxford, UK: University Press; 1995.